Alan Watts: “If you get the message, hang up the phone. For psychedelic drugs are simply instruments, like microscopes, telescopes, and telephones. The biologist does not sit with eye permanently glued to the microscope, he goes away and works on what he has seen.”
The therapeutic process
Psychedelic-assisted therapies typically involves ‘talk-therapy’ alongside the ingestion of a classical psychedelic such as psilocybin, LSD, or ayahuasca. Researchers and clinicians often describe three distinct therapy phases:
- preparation,
- the acute psychedelic experience,
- and integration.
The non-psychedelic elements of this approach are essential for both effectiveness and safety.
These 3 phases are illustrated in the timeline below.
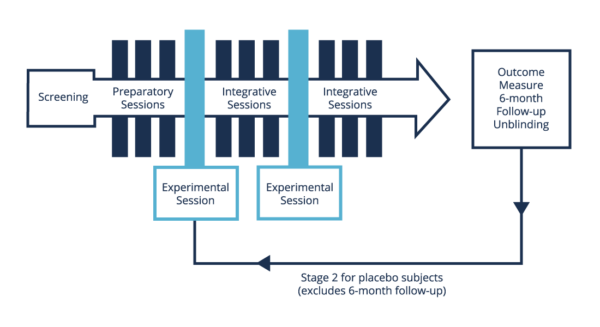
Various approaches to preparation have been developed, from diet to psychotherapy. In clinical trials, participants will typically attend a number of talk-therapy sessions with a trained therapist who will be in attendance during the psychedelic session. A therapeutic alliance is developed during this time, and the nature of the individual’s struggle is explored.
The therapist will prepare the patient for the psychedelic session in a number of ways, with a particular emphasis on curiosity, and ways to remain open to challenging experiences (“If you see a door, go through it”; “If you meet something scary, walk towards it and ask, ‘what do you have to teach me?’”). While challenging experiences are considered by many who work in the field to be integral to the therapeutic and personal benefits that follow, the so called ‘bad trip’ is borne out of an attempt to avoid the experience, and can be mitigated by an open and trusting approach.
During the psychedelic session, ‘set’ and ‘setting’ are considered paramount. ‘Set’ refers to mind-set, a complex mix of more transient phenomena like expectation and mood, and more enduring phenomena like personality and past experience. ‘Setting’ refers to the context or environment in which the session takes place, including basic factors like the comfort and aesthetic quality of the room, and more complex factors like the quality of the relationship with the clinicians and the mood they help to set. Whilst many modern clinical trials occur within hospitals or research institutes, the session rooms are made to appear as comfortable living rooms (see image 1). There are typically two therapists in attendance. The patient can sit or lie on a couch, is often encouraged to wear eyeshades, and sometimes listen to a carefully-selected playlist of music. Oral ingestion of a capsule of synthesised psychedelic compound (e.g., psilocybin) is the most common route of administration, and the session will typically last for about 8 hours.
A common therapeutic approach during psychedelic sessions is to be non-directive: attentive but usually silent, supporting the emerging process, offering assistance and guidance if needed, listening and responding to the patient when they speak, with little analysis of the material. In some trials, a single high-dose psychedelic session occurs (usually 20-30 mg per 70 kg body weight); in others, there are two or three high-dose sessions. Many trials are also placebo-controlled, wherein the patient will usually have one placebo session – sometimes a very low dose of the psychedelic, sometimes an ‘active placebo’ that produces some noticeable somatic effects – in addition to their high-dose session(s).
Immediately after the psychedelic session and in the following days, a process of integration is facilitated by the therapist. During these conversations, the patient has the opportunity to process, make sense of, and give meaningful expression to their psychedelic experience.
The psychedelic experience
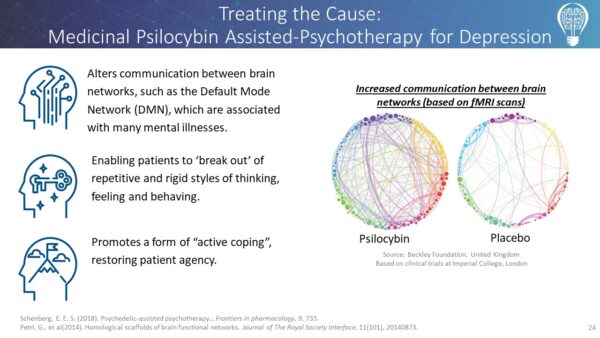
Classical psychedelics appear to produce many of their effects through the activation of a specific Serotonin receptor (5HT2A) in the brain. Numerous complex changes in brain activity occur following ingestion of a psychedelic, from reductions in activity in some areas (like the Default Mode Network, which is associated with mind-wandering, thinking about the past or future, and thinking about yourself), to alterations to the way different areas connect to each other (for example, areas of the brain that typically don’t interact much begin to work together). Much of what psychedelics do to brain activity remains to be investigated. What psychedelics do to the mind is also of central relevance to clinical research.
The ‘psychedelic experience’ is certainly not consistent across different people and the range of experiences and responses is wide. However, with specific constraints on ‘set’ and ‘setting’ – as is the case within modern clinical trials – certain subjective features occur for many people in a surprisingly reliable way. These include increased empathy for others; increased compassion for oneself; profound and novel insights about one’s character or life or the world; feelings of deep connectedness with other people or other things; a sense of meaningfulness; a reduced sense of one’s Self, its permanence, and its boundaries; and in some cases, a completely other-worldly experience often referred to as ‘mystical’. Psychedelic experiences entail an ‘altered state of consciousness’, a shift in the fundamental nature of one’s experience that is often startling, and difficult to imagine, much less describe. A common feature of these experiences is that the accompanying insights and perspectives are felt to be more reliable, more ‘true’ or ‘wise’, than one’s usual understanding. Further, the ‘authority’ of these novel perspectives tends to endure well beyond the acute stages of the psychedelic session.

What is the clinical evidence?
Internationally, there has been a resurgence of research into psychedelics at universities such as Harvard, Johns Hopkins, New York University, Stanford, Imperial College London, and the University of Zurich. Hundreds of well-controlled clinical trials have yielded promising results. The new data confirms that psychedelic-assisted psychotherapies frequently lead to remission from certain mental illnesses within a few doses, when administered with proper psychotherapeutic support before, during and after treatments. The proportion of participants who show positive clinical improvements, and the degree to which they improve, are substantially higher than clinical outcomes associated with currently available treatments. Psilocybin-assisted therapy can lead to remission in 60-80% of cases of anxiety and depression, whereas current existing treatments lead to remission in a maximum of 30-35% of cases.
How effective are psychedelics compared with current treatments?
Current drug and talk therapies for depression and anxiety achieve remission in only 30-35% of cases, with high rates of sub-diagnostic symptoms and relapse. In a trial involving participants who had failed to respond to several different drug and talk therapies, psilocybin-assisted therapy substantially reduced depressive symptoms in over 65% of these ‘treatment-resistant’ patients.
In a trial using psilocybin-assisted therapy for smoking cessation, 80% of patients had quit smoking six months after the therapeutic sessions, and after one year, that figure was still at 67%. Typically, the current “gold-standard” smoking cessation treatments with similarly addicted participants can hope to achieve around a 20% quit rate at follow-up.
PTSD is notoriously hard to treat. Only 5-10% sufferers experience remission from existing treatments. In recent Phase 3 trials conducted by MAPS, MDMA-assisted therapy led to remission in 67% of PTSD patients who had not previously responded to standard treatments after just 3 medicinal doses of MDMA in combination with a short course of psychotherapy. 88% of patients experienced a clinically meaningful reduction in symptoms. The patients had been suffering with PTSD for an average of 14 years.
MDMA and psilocybin have been granted “Breakthrough Therapy” designation, expediting research and the transition to prescription medicine due to their potential superiority over existing treatments.
Footnotes
- MDMA is not a classical psychedelic, but is associated with various ‘psychedelic effects’ and often discussed among the classical psychedelics.
- Johnson, M et al. (2014). 5-HT2AR agonist psilocybin in the treatment of tobacco addiction. Journal of Psychopharmacology, 28-11:983-992.
- Carhart-Harris et al. (2016). Psilocybin with psychological support for treatment-resistant depression. The Lancet, 3-7:619-627.
- Griffiths, R. R. et al. (2016). Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: A randomized double-blind trial. Journal of psychopharmacology, 30(12), 1181-1197.
- Ross et al. (2016). Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. Journal of Psychopharmacology, 30-12:1165-1180.
- M.C. Mithoefer, T.M. Wagner, A.T. Mithoefer, L. Jerome, R. Doblin, The safety and efficacy of ±3,4-methylenedioxymethamphetamine-assisted psychotherapy in subjects with chronic, treatment-resistant posttraumatic stress disorder: the first randomized controlled pilot study, J. Psychopharmacol. 25 (4) (2011) 439–452.
